The treatment of infectious disease often becomes a race against time. Doctors desperately order test after test to determine the cause of a patient’s infection. They ask about recent travel destinations or interactions with animals, trying to narrow down possible pathogen exposures. Meanwhile, the patient’s condition continues to deteriorate.
Can artificial intelligence change this scenario? After all, AI is transforming clinical decisionmaking, personalized disease treatment, imaging analysis, drug development and much more. What if it could also transform the way doctors approach infectious disease?
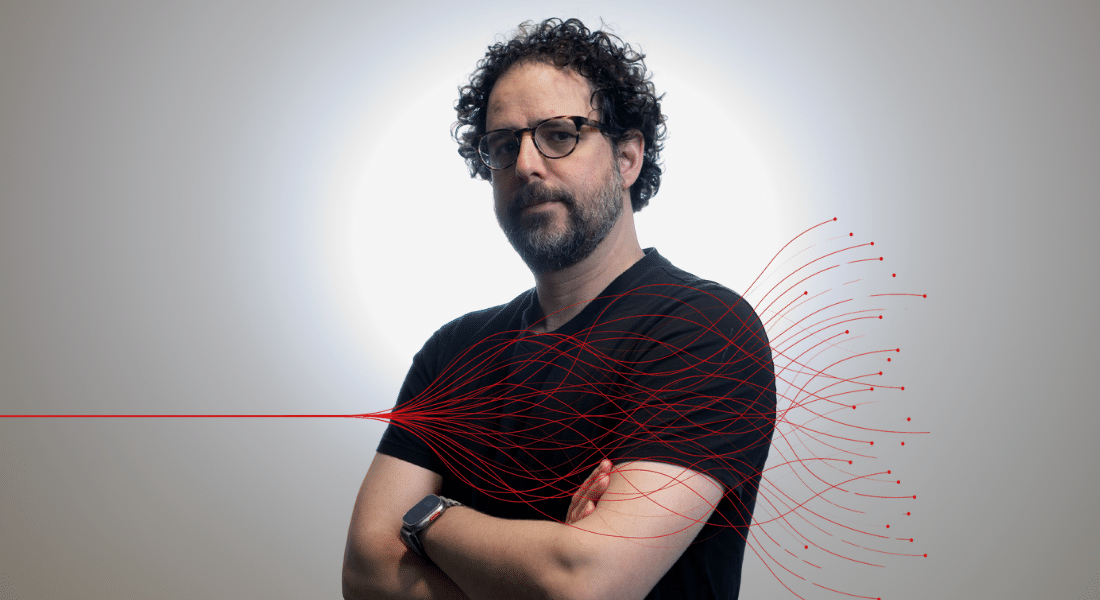
It turns out, thanks to the trailblazing work of Sivan Bercovici and his team, it already is. Bercovici, a computer scientist and former Azrieli Graduate Studies Fellow, is leading the team pioneering a new AI-enabled test that screens samples for more than 1,000 human pathogens all at once. Known as the Karius Test, the technology can help physicians reduce the time it takes to diagnose patients with an infection. Published literature by a growing community of healthcare providers, as well as by Bercovici and his colleagues, have demonstrated its diagnostic value where other tests have failed. More than 500 U.S. hospitals already use the test, with the Karius corporate facility in Redwood City, California, having processed nearly 90,000 cases so far.
“When cells in your body die, DNA is spilled into the bloodstream,” says Bercovici. This also happens when bacteria, fungi, parasites or viruses die — even when an infection is worsening, as some of these infecting cells still break down and release their DNA. “The test we’ve developed, offered as an approved laboratory developed test service, is the only approved test that can detect and interpret that signal.”
For the last 20 years, Bercovici has been studying the intersection between human health and machine learning. During his PhD work at Technion–Israel Institute of Technology, he focused on developing methods to discover genes that contribute to diseases, including prostate cancer, multiple sclerosis and end-stage kidney disease. In one example, using an AI program that analyzed genetic information taken from hundreds of patients, Bercovici helped pinpoint mutations in a single gene that explained why African Americans have a four-fold risk of end-stage kidney disease compared to Americans of European descent.
“Some 15 years later, there are major practical diagnostic and therapeutic advances that have come out of this work,” says Karl Skorecki, professor emeritus and former dean of the Azrieli Faculty of Medicine at Bar-Ilan University, with whom Bercovici collaborated on kidney disease research.
After completing his PhD, Bercovici continued to apply AI to genetic analysis in his postdoctoral work, and, later, as a senior research scientist at Stanford University. “One thing about hanging out at Stanford is that you get to see really exciting stuff that is very far from commercialization,” says Bercovici. “It’s a glimpse into the future.”